Neuroblastoma Treatment In India
Introduction
Neuroblastoma is the fourth most common malignancy of childhood, preceded by leukemias, CNS tumors, and lymphomas. Neuroblastoma is the most common intra-abdominal malignancy of infancy and the most common extracranial solid tumor of childhood. It is a poorly differentiated neoplasm derived from neural crest cells that typically affects infants and young children. Neuroblastoma is one of the small, blue, round cell tumors of childhood. Other such tumors include Ewing sarcoma, non-Hodgkin lymphoma, primitive neuroectodermal tumors, and undifferentiated soft tissue sarcoma (rhabdomyosarcoma).
History of the Procedure
 Virchow first described neuroblastoma in 1864; at that time, it was referred to as a glioma.In 1891, Marchand histologically linked neuroblastoma to sympathetic ganglia.2 More substantial evidence of the neural origins of neuroblastoma became apparent in 1914, when Herxheimer showed that fibrils of the tumor stained positively with special neural silver stains.
Virchow first described neuroblastoma in 1864; at that time, it was referred to as a glioma.In 1891, Marchand histologically linked neuroblastoma to sympathetic ganglia.2 More substantial evidence of the neural origins of neuroblastoma became apparent in 1914, when Herxheimer showed that fibrils of the tumor stained positively with special neural silver stains.
In 1927, Cushing and Wolbach further characterized neuroblastoma by describing the transformation of malignant neuroblastoma into its benign counterpart, ganglioneuroma Everson and Cole reported that this type of transformation is rare in children older than 6 months.In 1957, Mason published a report of a child with neuroblastoma whose urine contained pressor amines.This discovery further contributed to the understanding of neuroblastoma and its possible sympathetic neural origin.
Spontaneous regression of microscopic clusters of neuroblastoma cells, called neuroblastoma in situ, was noted to occur quite commonly. According to Beckwith and Perrin in 1963, regression occurs nearly 40 times more often than clinically apparent neuroblastoma.
Problem
Neuroblastoma is a malignant neural tumor that affects very young children. Its presentation varies depending on the primary site of origin, metastatic burden, and metabolically active by-products. It is unique in several different ways. It has a documented spontaneous rate of resolution and is also one of the few tumors in which the surgical capsule can be violated, leaving residual tumor, and a good outcome might still be achieved.
Frequency
Clinical frequency is approximately 1 case per 8000-10,000 children, which would predict approximately 600 new cases of neuroblastoma in the United States each year. Neuroblastoma is more common in whites and is slightly more prevalent in boys than in girls (male-to-female ratio of 1.3:1). The typical age at diagnosis is younger than that for Wilms tumor. More than one third of cases (36%) are diagnosed in children younger than 1 year. Seventy-nine percent of cases are diagnosed are children younger than 4 years, and 97% are diagnosed by age 10 years. Neuroblastoma is thought to occur sporadically, with 1-2% of cases thought to be familial.
Etiology
The actual etiology of the tumor is obscure. Environmental and paternal exposures linked to neuroblastoma have not been identified. Embryologically, tumors of the sympathetic nervous system differentiate along 2 distinct pathways, either the pheochromocytoma line or the sympathoblastoma line. The sympathoblastomas, also called neurocristopathies, include the well-differentiated ganglioneuroma, the moderately differentiated ganglioneuroblastoma, and the malignant neuroblastoma. All of these tumors arise from primordial neural crest cells, which ultimately populate the sympathetic chain and the adrenal medulla.
Pathophysiology
According to Knudson and Strong (1972), 20% of neuroblastomas are inherited in an autosomal dominant pattern.Twenty percent of this cohort has bilateral or multifocal primary tumors. Various karyotypic abnormalities occur, but a deletion of the short arm of chromosome 1 is found in 70-80% of all patients with neuroblastomas.
Malignant transformation and maintenance of the dedifferentiated state of neural crest cells may result from failure of those cells to respond to normal signals that are responsible for normal morphologic differentiation. The factors involved in the cascade of events are poorly understood but most likely involve one or more ligand-receptor pathways. One of the most studied and most popular pathways is the nerve growth factor (NGF) and its receptor (NGFR). The dedifferentiated state of neuroblastoma leads to the variable presentations commonly observed in patients with neuroblastoma.
Presentation
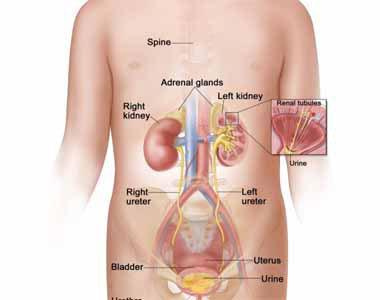
Neuroblastoma has been called the great mimicker because of its myriad clinical presentations related to the site of the primary tumor, metastatic disease, and its metabolic tumor by-products. Sixty-five percent of primary neuroblastomas occur in the abdomen, with most of these occurring in the adrenal gland. As a result, most children present with abdominal symptoms, such as fullness or distension.
Obtaining a complete history and physical examination are paramount to an accurate diagnosis and subsequent management of neuroblastoma. Eliciting a history of the child's general appearance, recent trauma, changes in appetite and weight, and recurrent abdominal pain is important. Symptoms are usually related to either an abdominal mass or bone pain secondary to metastatic neuroblastoma. Reports of fatigue, bone pain, and changes in bowel or bladder habits may contribute to an accurate diagnosis. Physical findings might include hepatomegaly; blanching subcutaneous nodules; or a large, irregular, firm abdominal mass.
Typically, children with localized disease are asymptomatic, whereas children with disseminated neuroblastoma are generally sick and may have systemic manifestations, including unexplained fevers, weight loss, anorexia, failure to thrive, general malaise, irritability, and bone pain. The most common finding upon physical examination is a nontender, firm, irregular abdominal mass that crosses the midline. In contrast, children who present with Wilms tumor have a smooth mobile flank mass that typically does not cross the midline.
At diagnosis, the site of neuroblastoma is predictably age-dependent. Infants often present with compression of the sympathetic ganglia in the thoracic region, which might result, for example, in Horner syndrome (myosis, anhydrosis, and ptosis) or superior vena cava syndrome. Older children typically present with abdominal symptoms because, as stated above, more than 40% of neuroblastomas are adrenal in origin. Children who are preschool aged should have working differential diagnoses for an abdominal mass, including lymphoma, hepatoblastoma, rhabdomyosarcoma, renal cell carcinoma, and neuroblastoma.
More than 50% of patients who present with neuroblastoma have metastatic disease. The fact that many other syndromes related to metastatic neuroblastoma are also common in these patients is not surprising.
For example, Pepper syndrome occurs in infants with overwhelming metastatic neuroblastoma of the liver that results in respiratory compromise. Described by William Pepper in 1901, Pepper syndrome was identified as a localized primary tumor and metastatic disease limited to the skin, liver, and bone marrow in infants. Pepper syndrome has since been associated with stage 4S neuroblastoma, a unique entity that occurs only in infants younger than 1 year. Pepper syndrome generally confers a better prognosis, as it is associated with spontaneous regression. Some infants with stage 4S neuroblastoma, however, die of massive hepatomegaly, respiratory failure, and overwhelming sepsis.
"Blueberry muffin" babies are infants in whom neuroblastoma has metastasized to random subcutaneous sites. When provoked, the nodules become intensely red and subsequently blanch for several minutes thereafter. The response is probably secondary to the release of vasoconstrictive metabolic tumor by-products. These nodules can be diagnostic of neuroblastoma, but leukemic infiltrates that metastasize to the skin should be considered in the differential diagnoses when these children are evaluated.
Widespread metastasis of neuroblastoma to the bone may result in Hutchinson syndrome, which results in bone pain with consequent limping and pathologic fractures. Neuroblastomas that arise in the paraspinal ganglia may invade through the neural foramina, compress the spinal cord, and subsequently cause paralysis.
Infrequently, neuroblastoma can become metastatic to the retrobulbar region, leading to rapidly progressive, unilateral, painless proptosis; periorbital edema; and ecchymosis of the upper lid. This lesion often can be confused with trauma or child abuse.
Most neuroblastomas produce catecholamines as metabolic by-products, which result in some of the most interesting presentations observed in children with neuroblastoma. For example, Kerner-Morrison syndrome causes intractable secretory diarrhea, resulting in hypovolemia, hypokalemia, and prostration. This syndrome is caused by vasoactive intestinal peptide (VIP) tumor secretion and is more commonly associated with ganglioneuroblastoma or ganglioneuroma. Kerner-Morrison syndrome typically resolves following the complete removal of the tumor.
A wide variety of neoplastic and nonneoplastic lesions might be confused with neuroblastoma. Wilms tumor and lymphoma are 2 malignant lesions that might be mistaken for neuroblastoma. The nonneoplastic lesions are particularly confusing, especially in the 5-11% of neuroblastomas that do not produce catecholamine metabolic by-products. Nonmalignant lesions that might be confused with neuroblastoma include ganglioneuroma and congenital mesoblastic nephroma.
Indications
In 1988, the Pediatric Oncology Group (POG) released a prospective study that revealed that 89% of patients with localized neuroblastoma who were treated by surgical extirpation had only 2 years of disease-free survival.Additionally, chemotherapy appeared to offer no advantage when residual disease was present in these patients. Thus, in patients with low-stage favorable disease, surgery is the mainstay of therapy. The primary goals of surgery are (1) to determine an accurate diagnosis, (2) to completely remove all of the primary tumor, (3) to provide accurate surgical staging, (4) to offer adjuvant therapy for delayed primary surgery, and (5) to remove residual disease with second-look surgery.