Melanoma
Introduction:
Melanoma* is the most serious type of cancer of the skin. Each year in the United States, more than 53,600 people learn they have melanoma.
In some parts of the world, especially among Western countries, melanoma is becoming more common every year. In the United States, for example, the percentage of people who develop melanoma has more than doubled in the past 30 year
What Is Melanoma?
Melanoma is a type of skin cancer. It begins in cells in the skin called melanocytes. To understand melanoma, it is helpful to know about the skin and about melanocytes—what they do, how they grow, and what happens when they become cancerous
The Skin
The skin is the body’s largest organ. It protects against heat, sunlight, injury, and infection. It helps regulate body temperature, stores water and fat, and produces vitamin D.
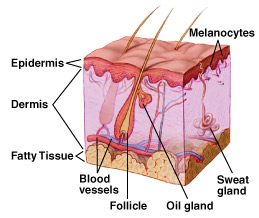
The skin has two main layers: the outer epidermis and the inner dermis.
- The epidermis is mostly made up of flat, scalelike cells called squamous cells. Round cells called basal cells lie under the squamous cells in the epidermis. The lower part of the epidermis also contains melanocytes.
- The dermis contains blood vessels, lymph vessels, hair follicles, and glands. Some of these glands produce sweat, which helps regulate body temperature. Other glands produce sebum, an oily substance that helps keep the skin from drying out. Sweat and sebum reach the skin’s surface through tiny openings called pores.
Melanocytes and Moles
Melanocytes produce melanin, the pigment that gives skin its natural color. When skin is exposed to the sun, melanocytes produce more pigment, causing the skin to tan, or darken.
Sometimes, clusters of melanocytes and surrounding tissue form no cancerous growths called moles. (Doctors also call a mole a nevus; the plural is nevi.) Moles are very common. Most people have between 10 and 40 moles. Moles may be pink, tan, brown, or a color that is very close to the person’s normal skin tone. People who have dark skin tend to have dark moles. Moles can be flat or raised. They are usually round or oval and smaller than a pencil eraser. They may be present at birth or may appear later on—usually before age 40. They tend to fade away in older people. When moles are surgically removed, they normally do not return
Understanding Cancer
Cancer begins in cells, the building blocks that make up tissues. Tissues make up the organs of the body. Normally, cells grow and divide to form new cells as the body needs them. When cells grow old, they die, and new cells take their place.
Sometimes this orderly process goes wrong. New cells form when the body does not need them, and old cells do not die when they should. These extra cells can form a mass of tissue called a growth or tumor. Not all tumors are cancer.
Tumors can be benign or malignant:
- Benign tumors are not cancer:
- They are rarely life threatening.
- Usually, benign tumors can be removed, and they seldom grow back.
- Cells from benign tumors do not spread to tissues around them or to other parts of the body.
- Malignant tumors are cancer:
- They are generally more serious and may be life threatening.
- Malignant tumors usually can be removed, but they can grow back.
- Cells from malignant tumors can invade and damage nearby tissues and organs. Also, cancer cells can break away from a malignant tumor and enter the bloodstream or lymphatic system. That is how cancer cells spread from the original cancer (the primary tumor) to form new tumors in other organs. The spread of cancer is called metastasis. Different types of cancer tend to spread to different parts of the body
Melanoma
Melanoma occurs when melanocytes (pigment cells) become malignant. Most pigment cells are in the skin; when melanoma starts in the skin, the disease is called cutaneous melanoma. Melanoma may also occur in the eye (ocular melanoma or intraocular melanoma). Rarely, melanoma may arise in the meninges, the digestive tract, lymph nodes, or other areas where melanocytes are found. Melanomas that begin in areas other than the skin are not discussed in this booklet.
Melanoma is one of the most common cancers. The chance of developing it increases with age, but this disease affects people of all ages. It can occur on any skin surface. In men, melanoma is often found on the trunk (the area between the shoulders and the hips) or the head and neck. In women, it often develops on the lower legs. Melanoma is rare in black people and others with dark skin. When it does develop in dark-skinned people, it tends to occur under the fingernails or toenails, or on the palms or soles.
When melanoma spreads, cancer cells may show up in nearby lymph nodes. Groups of lymph nodes are found throughout the body. Lymph nodes trap bacteria, cancer cells, or other harmful substances that may be in the lymphatic system. If the cancer has reached the lymph nodes, it may mean that cancer cells have spread to other parts of the body such as the liver, lungs, or brain. In such cases, the cancer cells in the new tumor are still melanoma cells, and the disease is called metastatic melanoma, not liver, lung, or brain cancer
Melanoma: Who’s at Risk?
No one knows the exact causes of melanoma. Doctors can seldom explain why one person gets melanoma and another does not.
However, research has shown that people with certain risk factors are more likely than others to develop melanoma. A risk factor is anything that increases a person’s chance of developing a disease. Still, many who do get this disease have no known risk factors.
Studies have found the following risk factors for melanoma:
- Dysplastic nevi: Dysplastic nevi are more likely than ordinary moles to become cancerous. Dysplastic nevi are common, and many people have a few of these abnormal moles. The risk of melanoma is greatest for people who have a large number of dysplastic nevi. The risk is especially high for people with a family history of both dysplastic nevi and melanoma.
- Many (more than 50) ordinary moles: Having many moles increases the risk of developing melanoma.
- Fair skin: Melanoma occurs more frequently in people who have fair skin that burns or freckles easily (these people also usually have red or blond hair and blue eyes) than in people with dark skin. White people get melanoma far more often than do black people, probably because light skin is more easily damaged by the sun.
- Personal history of melanoma or skin cancer: People who have been treated for melanoma have a high risk of a second melanoma. Some people develop more than two melanomas. People who had one or more of the common skin cancers (basal cell carcinoma or squamous cell carcinoma) are at increased risk of melanoma.
- Family history of melanoma: Melanoma sometimes runs in families. Having two or more close relatives who have had this disease is a risk factor. About 10 percent of all patients with melanoma have a family member with this disease. When melanoma runs in family, all family members should be checked regularly by a doctor.
- Weakened immune system: People whose immune system is weakened by certain cancers, by drugs given following organ transplantation, or by HIV are at increased risk of developing melanoma.
- Severe, blistering sunburns: People who have had at least one severe, blistering sunburn as a child or teenager are at increased risk of melanoma. Because of this, doctors advise that parents protect children’s skin from the sun. Such protection may reduce the risk of melanoma later in life. Sunburns in adulthood are also a risk factor for melanoma.
- Ultraviolet (UV) radiation: Experts believe that much of the worldwide increase in melanoma is related to an increase in the amount of time people spend in the sun. This disease is also more common in people who live in areas that get large amounts of UV radiation from the sun. In the United States, for example, melanoma is more common in Texas than in Minnesota, where the sun is not as strong. UV radiation from the sun causes premature aging of the skin and skin damage that can lead to melanoma. Artificial sources of UV radiation, such as sunlamps and tanning booths, also can cause skin damage and increase the risk of melanoma. Doctors encourage people to limit their exposure to natural UV radiation and to avoid artificial sources.
Doctors recommend that people take steps to help prevent and reduce the risk of melanoma caused by UV radiation:
- Avoid exposure to the midday sun (from 10 a.m. to 4 p.m.) whenever possible. When your shadow is shorter than you are, remember to protect yourself from the sun.
- If you must be outside, wear long sleeves, long pants, and a hat with a wide brim.
- Protect yourself from UV radiation that can penetrate light clothing, windshields, and windows.
- Protect yourself from UV radiation reflected by sand, water, snow, and ice.
- Help protect your skin by using a lotion, cream, or gel that contains sunscreen. Many doctors believe sunscreens may help prevent melanoma, especially sunscreens that reflect, absorb, and/or scatter both types of ultraviolet radiation. These sunscreen products will be labeled with “broad-spectrum coverage.” Sunscreens are rated in strength according to a sun protection factor (SPF). The higher the SPF, the more sunburn protection is provided. Sunscreens with an SPF value of 2 to 11 provide minimal protection against sunburns. Sunscreens with an SPF of 12 to 29 provide moderate protection. Those with an SPF of 30 or higher provide the most protection against sunburn.
- Wear sunglasses that have UV-absorbing lenses. The label should specify that the lenses block at least 99 percent of UVA and UVB radiation. Sunglasses can protect both the eyes and the skin around the eyes.
People who are concerned about developing melanoma should talk with their doctor about the disease, the symptoms to watch for, and an appropriate schedule for checkups. The doctor’s advice will be based on the person’s personal and family history, medical history, and other risk factors
Signs and Symptoms
Often, the first sign of melanoma is a change in the size, shape, color, or feel of an existing mole. Most melanomas have a black or blue-black area. Melanoma also may appear as a new mole. It may be black, abnormal, or “ugly looking.”
If you have a question or concern about something on your skin, see your doctor. Do not use the following pictures to try to diagnose it yourself. Pictures are useful examples, but they cannot take the place of a doctor’s examination.
Thinking of “ABCD” can help you remember what to watch for:
- Asymmetry—The shape of one half does not match the other.
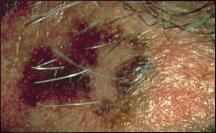
- Border—The edges are often ragged, notched, blurred, or irregular in outline; the pigment may spread into the surrounding skin.

- Color—The color is uneven. Shades of black, brown, and tan may be present. Areas of white, grey, red, pink, or blue also may be seen.

- Diameter—There is a change in size, usually an increase. Melanomas are usually larger than the eraser of a pencil (1/4 inch or 5 millimeters).

- Melanomas can vary greatly in how they look. Many show all of the ABCD features. However, some may show changes or abnormalities in only one or two of the ABCD features.

Melanomas in an early stage may be found when an existing mole changes slightly, for example, when a new black area forms. Newly formed fine scales and itching in a mole also are common symptoms of early melanoma. In more advanced melanoma, the texture of the mole may change. For example, it may become hard or lumpy. Melanomas may feel different from regular moles. More advanced tumors may itch, ooze, or bleed. But melanomas usually do not cause pain.
A skin examination is often part of a routine checkup by a health care provider. People also can check their own skin for new growths or other changes. Changes in the skin, such as a change in a mole, should be reported to the health care provider right away. The person may be referred to a dermatologist, a doctor who specializes in diseases of the skin.
Melanoma can be cured if it is diagnosed and treated when the tumor is thin and has not deeply invaded the skin. However, if a melanoma is not removed at its early stages, cancer cells may grow downward from the skin surface and invade healthy tissue. When a melanoma becomes thick and deep, the disease often spreads to other parts of the body and is difficult to control.
People who have had melanoma have a high risk of developing a new melanoma. People at risk for any reason should check their skin regularly and have regular skin exams by a health care provider
Dysplastic Nevi
Some people have certain abnormal-looking moles (called dysplastic nevi or atypical moles) that are more likely than normal moles to develop into melanoma. Most people with dysplastic nevi have just a few of these abnormal moles; some people have many. People with dysplastic nevi and their health care provider should examine these moles regularly to watch for changes.
Dysplastic nevi often look very much like melanoma. Doctors with special training in skin diseases are in the best position to decide whether an abnormal-looking mole should be closely watched or removed and checked for cancer.
In some families, many members have a large number of dysplastic nevi, and some have had melanoma. Members of these families have a very high risk of melanoma. Doctors often recommend that they have frequent checkups (every 3 to 6 months) so that any problems can be detected early. The doctor may take pictures of a person’s skin to help show when changes occur.





































