Lung Cancer, Non Small Cell
Introduction:
This page has important information about cancer* that begins in the lung. It tells about diagnosis, staging, treatment, and comfort care. Learning about the medical care for people with lung cancer can help you take an active part in making choices about your own care.
The Lungs
Your lungs are a pair of large organs in your chest. They are part of your respiratory system. Air enters your body through your nose or mouth. It passes through your windpipe (trachea) and through each bronchus, and goes into your lungs.
When you breathe in, your lungs expand with air. This is how your body gets oxygen.
When you breathe out, air goes out of your lungs. This is how your body gets rid of carbon dioxide.
Your right lung has three parts (lobes). Your left lung is smaller and has two lobes.
A thin tissue (the pleura) covers the lungs and lines the inside of the chest. Between the two layers of the pleura is a very small amount of fluid (pleural fluid). Normally, this fluid does not build up.
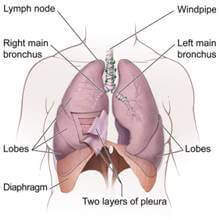
This is a picture of the lungs and nearby tissues
Cancer Cells
Cancer begins in cells, the building blocks that make up tissues. Tissues make up the organs of the body.
Normal, healthy cells grow and divide to form new cells as the body needs them. When normal cells grow old or become damaged, they die, and new cells take their place.
Sometimes, this orderly process goes wrong. New cells form when the body does not need them, and old or damaged cells do not die as they should. The build-up of extra cells often forms a mass of tissue called a growth or tumor.
Tumor cells can be benign (not cancer) or malignant (cancer). Benign tumor cells are usually not as harmful as malignant tumor cells:
- Benign lung tumors
- are rarely a threat to life
- usually do not need to be removed
- do not invade the tissues around them
- do not spread to other parts of the body
- Malignant lung tumors
- may be a threat to life
- may grow back after being removed
- can invade nearby tissues and organs
- can spread to other parts of the body
Cancer cells spread by breaking away from the original tumor. They enter blood vessels or lymph vessels, which branch into all the tissues of the body. The cancer cells attach to other organs and form new tumors that may damage those organs. The spread of cancer is called metastasis.
Risk Factors
Doctors cannot always explain why one person develops lung cancer and another does not. However, we do know that a person with certain risk factors may be more likely than others to develop lung cancer. A risk factor is something that may increase the chance of developing a disease.
Studies have found the following risk factors for lung cancer:
- Tobacco smoke: Tobacco smoke causes most cases of lung cancer. It's by far the most important risk factor for lung cancer. Harmful substances in smoke damage lung cells. That's why smoking cigarettes, pipes, or cigars can cause lung cancer and why secondhand smoke can cause lung cancer in nonsmokers. The more a person is exposed to smoke, the greater the risk of lung cancer.
- Radon: Radon is a radioactive gas that you cannot see, smell, or taste. It forms in soil and rocks. People who work in mines may be exposed to radon. In some parts of the country, radon is found in houses. Radon damages lung cells, and people exposed to radon are at increased risk of lung cancer. The risk of lung cancer from radon is even higher for smokers. For more information, see the NCI fact sheet Radon and Cancer.
- Asbestos and other substances: People who have certain jobs (such as those who work in the construction and chemical industries) have an increased risk of lung cancer. Exposure to asbestos, arsenic, chromium, nickel, soot, tar, and other substances can cause lung cancer. The risk is highest for those with years of exposure. The risk of lung cancer from these substances is even higher for smokers.
- Air pollution: Air pollution may slightly increase the risk of lung cancer. The risk from air pollution is higher for smokers.
- Family history of lung cancer: People with a father, mother, brother, or sister who had lung cancer may be at slightly increased risk of the disease, even if they don't smoke.
- Personal history of lung cancer: People who have had lung cancer are at increased risk of developing a second lung tumor.
- Age over 65: Most people are older than 65 years when diagnosed with lung cancer.
Researchers have studied other possible risk factors. For example, having certain lung diseases (such as tuberculosis or bronchitis) for many years may increase the risk of lung cancer. It's not yet clear whether having certain lung diseases is a risk factor for lung cancer.
People who think they may be at risk for developing lung cancer should talk to their doctor. The doctor may be able to suggest ways to reduce their risk and can plan an appropriate schedule for checkups. For people who have been treated for lung cancer, it's important to have checkups after treatment. The lung tumor may come back after treatment, or another lung tumor may develop.
How To Quit Smoking
Quitting is important for anyone who smokes tobacco -- even people who have smoked for many years. For people who already have cancer, quitting may reduce the chance of getting another cancer. Quitting also can help cancer treatments work better.
There are many ways to get help:
- Ask your doctor about medicine or nicotine replacement therapy, such as a patch, gum, lozenge, nasal spray, or inhaler. Your doctor can suggest a number of treatments that help people quit.
- Ask your doctor to help you find local programs or trained professionals who help people stop using tobacco.
Screening
Screening tests may help doctors find and treat cancer early. They have been shown to be very helpful in some cancers such as breast cancer. Currently, there is no generally accepted screening test for lung cancer. Several methods of detecting lung cancer have been studied as possible screening tests. The methods under study include tests of sputum (mucus brought up from the lungs by coughing), chest x-rays, or spiral (helical) CT scans. You can read more about these tests in the Diagnosis section.
However, screening tests have risks. For example, an abnormal x-ray result could lead to other procedures (such as surgery to check for cancer cells), but a person with an abnormal test result might not have lung cancer. Studies so far have not shown that screening tests lower the number of deaths from lung cancer. See "The Promise of Cancer Research" section for information about research studies of screening tests for lung cancer.
You may want to talk with your doctor about your own risk factors and the possible benefits and harms of being screened for lung cancer. Like many other medical decisions, the decision to be screened is a personal one. Your decision may be easier after learning the pros and cons of screening.
Symptoms
Early lung cancer often does not cause symptoms. But as the cancer grows, common symptoms may include:
- a cough that gets worse or does not go away
- breathing trouble, such as shortness of breath
- constant chest pain
- coughing up blood
- a hoarse voice
- frequent lung infections, such as pneumonia
- feeling very tired all the time
- weight loss with no known cause
Most often these symptoms are not due to cancer. Other health problems can cause some of these symptoms. Anyone with such symptoms should see a doctor to be diagnosed and treated as early as possible.