Breast Cancer Male
Introduction:
This page has important information about breast cancer.* Breast cancer is the most common type of cancer among women in this country (other than skin cancer). Each year, more than 211,000 American women learn they have this disease.
You will read about possible causes, screening, symptoms, diagnosis, treatment, and supportive care. You will also find ideas about how to cope with the disease.
Scientists are studying breast cancer to find out more about its causes. And they are looking for better ways to prevent, find, and treat it.
The Breasts
The breasts sit on the chest muscles that cover the ribs. Each breast is made of 15 to 20 lobes. Lobes contain many smaller lobules. Lobules contain groups of tiny glands that can produce milk. Milk flows from the lobules through thin tubes called ducts to the nipple. The nipple is in the center of a dark area of skin called the areola. Fat fills the spaces between the lobules and ducts.
The breasts also contain lymph vessels. These vessels lead to small, round organs called lymph nodes. Groups of lymph nodes are near the breast in the axilla (underarm), above the collarbone, in the chest behind the breastbone, and in many other parts of the body. The lymph nodes trap bacteria, cancer cells, or other harmful substances.
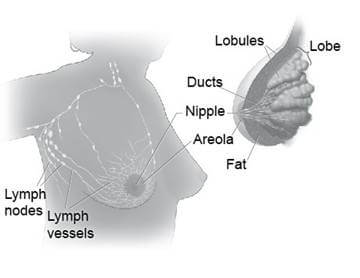 These pictures show the parts of the breast and the lymph nodes and lymph vessels near the breast
These pictures show the parts of the breast and the lymph nodes and lymph vessels near the breast
Understanding Cancer
Cancer begins in cells, the building blocks that make up tissues. Tissues make up the organs of the body.
Normally, cells grow and divide to form new cells as the body needs them. When cells grow old, they die, and new cells take their place.
Sometimes, this orderly process goes wrong. New cells form when the body does not need them, and old cells do not die when they should. These extra cells can form a mass of tissue called a growth or tumor.
Tumors can be benign or malignant:- Benign tumors are not cancer:
- Benign tumors are rarely life-threatening.
- Generally, benign tumors can be removed. They usually do not grow back.
- Cells from benign tumors do not invade the tissues around them.
- Cells from benign tumors do not spread to other parts of the body.
- Malignant tumors are cancer:
- Malignant tumors are generally more serious than benign tumors. They may be life-threatening.
- Malignant tumors often can be removed. But sometimes they grow back.
- Cells from malignant tumors can invade and damage nearby tissues and organs.
- Cells from malignant tumors can spread (metastasize) to other parts of the body. Cancer cells spread by breaking away from the original (primary) tumor and entering the bloodstream or lymphatic system. The cells invade other organs and form new tumors that damage these organs. The spread of cancer is called metastasis.
When breast cancer cells spread, the cancer cells are often found in lymph nodes near the breast. Also, breast cancer can spread to almost any other part of the body. The most common are the bones, liver, lungs, and brain. The new tumor has the same kind of abnormal cells and the same name as the primary tumor. For example, if breast cancer spreads to the bones, the cancer cells in the bones are actually breast cancer cells. The disease is metastatic breast cancer, not bone cancer. For that reason, it is treated as breast cancer, not bone cancer. Doctors call the new tumor "distant" or metastatic disease
Risk Factors
No one knows the exact causes of breast cancer. Doctors often cannot explain why one woman develops breast cancer and another does not. They do know that bumping, bruising, or touching the breast does not cause cancer. And breast cancer is not contagious. You cannot "catch" it from another person.
Research has shown that women with certain risk factors are more likely than others to develop breast cancer. A risk factor is something that may increase the chance of developing a disease.
Studies have found the following risk factors for breast cancer:
- Age: The chance of getting breast cancer goes up as a woman gets older. Most cases of breast cancer occur in women over 60. This disease is not common before menopause.
- Personal history of breast cancer: A woman who had breast cancer in one breast has an increased risk of getting cancer in her other breast.
- Family history: A woman's risk of breast cancer is higher if her mother, sister, or daughter had breast cancer. The risk is higher if her family member got breast cancer before age 40. Having other relatives with breast cancer (in either her mother's or father's family) may also increase a woman's risk.
- Certain breast changes: Some women have cells in the breast that look abnormal under a microscope. Having certain types of abnormal cells (atypical hyperplasia and lobular carcinoma in situ [LCIS]) increases the risk of breast cancer.
- Gene changes: Changes in certain genes increase the risk of breast cancer. These genes include BRCA1, BRCA2, and others. Tests can sometimes show the presence of specific gene changes in families with many women who have had breast cancer. Health care providers may suggest ways to try to reduce the risk of breast cancer, or to improve the detection of this disease in women who have these changes in their genes. NCI offers publications on gene testing.
- Reproductive and menstrual history:
- The older a woman is when she has her first child, the greater her chance of breast cancer.
- Women who had their first menstrual period before age 12 are at an increased risk of breast cancer.
- Women who went through menopause after age 55 are at an increased risk of breast cancer.
- Women who never had children are at an increased risk of breast cancer.
- Women who take menopausal hormone therapy with estrogen plus progestin after menopause also appear to have an increased risk of breast cancer.
- Large, well-designed studies have shown no link between abortion or miscarriage and breast cancer.
- Race: Breast cancer is diagnosed more often in white women than Latina, Asian, or African American women.
- Radiation therapy to the chest: Women who had radiation therapy to the chest (including breasts) before age 30 are at an increased risk of breast cancer. This includes women treated with radiation for Hodgkin's lymphoma. Studies show that the younger a woman was when she received radiation treatment, the higher her risk of breast cancer later in life.
- Breast density: Breast tissue may be dense or fatty. Older women whose mammograms (breast x-rays) show more dense tissue are at increased risk of breast cancer.
- Taking DES (diethylstilbestrol): DES was given to some pregnant women in the United States between about 1940 and 1971. (It is no longer given to pregnant women.) Women who took DES during pregnancy may have a slightly increased risk of breast cancer. The possible effects on their daughters are under study.
- Being overweight or obese after menopause: The chance of getting breast cancer after menopause is higher in women who are overweight or obese.
- Lack of physical activity: Women who are physically inactive throughout life may have an increased risk of breast cancer. Being active may help reduce risk by preventing weight gain and obesity.
- Drinking alcohol: Studies suggest that the more alcohol a woman drinks, the greater her risk of breast cancer.
Other possible risk factors are under study. Researchers are studying the effect of diet, physical activity, and genetics on breast cancer risk. They are also studying whether certain substances in the environment can increase the risk of breast cancer.
Many risk factors can be avoided. Others, such as family history, cannot be avoided. Women can help protect themselves by staying away from known risk factors whenever possible.
But it is also important to keep in mind that most women who have known risk factors do not get breast cancer. Also, most women with breast cancer do not have a family history of the disease. In fact, except for growing older, most women with breast cancer have no clear risk factors.
If you think you may be at risk, you should discuss this concern with your doctor. Your doctor may be able to suggest ways to reduce your risk and can plan a schedule for checkups
Screening
- Screening Mammogram
- Clinical Breast Exam
- Breast Self-Exam
Screening for breast cancer before there are symptoms can be important. Screening can help doctors find and treat cancer early. Treatment is more likely to work well when cancer is found early.
Your doctor may suggest the following screening tests for breast cancer:
- Screening mammogram
- Clinical breast exam
- Breast self-exam
You should ask your doctor about when to start and how often to check for breast cancer
Screening Mammogram
- Women in their 40s and older should have mammograms every 1 to 2 years. A mammogram is a picture of the breast made with x-rays.
- Women who are younger than 40 and have risk factors for breast cancer should ask their health care provider whether to have mammograms and how often to have them.
Mammograms can often show a breast lump before it can be felt. They also can show a cluster of tiny specks of calcium. These specks are called microcalcifications. Lumps or specks can be from cancer, precancerous cells, or other conditions. Further tests are needed to find out if abnormal cells are present.
If an abnormal area shows up on your mammogram, you may need to have more x-rays. You also may need a biopsy. A biopsy is the only way to tell for sure if cancer is present.
Mammograms are the best tool doctors have to find breast cancer early. However, mammograms are not perfect:
- A mammogram may miss some cancers. (The result is called a "false negative.")
- A mammogram may show things that turn out not to be cancer. (The result is called a "false positive.")
- Some fast-growing tumors may grow large or spread to other parts of the body before a mammogram detects them.
Mammograms (as well as dental x-rays, and other routine x-rays) use very small doses of radiation. The risk of any harm is very slight, but repeated x-rays could cause problems. The benefits nearly always outweigh the risk. You should talk with your health care provider about the need for each x-ray. You should also ask for shields to protect parts of your body that are not in the picture.
Clinical Breast Exam
During a clinical breast exam, your health care provider checks your breasts. You may be asked to raise your arms over your head, let them hang by your sides, or press your hands against your hips.
Your health care provider looks for differences in size or shape between your breasts. The skin of your breasts is checked for a rash, dimpling, or other abnormal signs. Your nipples may be squeezed to check for fluid.
Using the pads of the fingers to feel for lumps, your health care provider checks your entire breast, underarm, and collarbone area. A lump is generally the size of a pea before anyone can feel it. The exam is done on one side, then the other. Your health care provider checks the lymph nodes near the breast to see if they are enlarged.
A thorough clinical breast exam may take about 10 minutes.
Breast Self-Exam
You may perform monthly breast self-exams to check for any changes in your breasts. It is important to remember that changes can occur because of aging, your menstrual cycle, pregnancy, menopause, or taking birth control pills or other hormones. It is normal for breasts to feel a little lumpy and uneven. Also, it is common for your breasts to be swollen and tender right before or during your menstrual period.
You should contact your health care provider if you notice any unusual changes in your breasts.
Breast self-exams cannot replace regular screening mammograms and clinical breast exams. Studies have not shown that breast self-exams alone reduce the number of deaths from breast cancer.
You may want to ask the doctor the following questions about screening:
- Which tests do you recommend for me? Why? Do the tests hurt? Are there any risks?
- How much do mammograms cost? Will my health insurance pay for them?
- How soon after the mammogram will I learn the results?
- If the results show a problem, how will you learn if I have cancer?
Symptoms
Common symptoms of breast cancer include:
- A change in how the breast or nipple feels
- A lump or thickening in or near the breast or in the underarm area
- Nipple tenderness
- A change in how the breast or nipple looks
- A change in the size or shape of the breast
- A nipple turned inward into the breast
- The skin of the breast, areola, or nipple may be scaly, red, or swollen. It may have ridges or pitting so that it looks like the skin of an orange.
- Nipple discharge (fluid)
Early breast cancer usually does not cause pain. Still, a woman should see her health care provider about breast pain or any other symptom that does not go away. Most often, these symptoms are not due to cancer. Other health problems may also cause them. Any woman with these symptoms should tell her doctor so that problems can be diagnosed and treated as early as possible