Bile Duct Treatment India
 A bile duct is any of a number of long tube-like structures that carry bile. Bile, required for the digestion of food, is excreted by the liver into passages that carry bile toward the hepatic duct, which joins with the cystic duct (carrying bile to and from the gallbladder) to form the common bile duct, which opens into the intestine. The biliary tree (see below) is the whole network of various sized ducts branching through the liver.
A bile duct is any of a number of long tube-like structures that carry bile. Bile, required for the digestion of food, is excreted by the liver into passages that carry bile toward the hepatic duct, which joins with the cystic duct (carrying bile to and from the gallbladder) to form the common bile duct, which opens into the intestine. The biliary tree (see below) is the whole network of various sized ducts branching through the liver.
The path is as follows:
- Bile canaliculi
- Canals of Hering
- interlobular bile ducts
- intrahepatic bile ducts
- left and right hepatic ducts merge to form
- common hepatic duct exits liver and joins
- cystic duct (from gall bladder) forming
- common bile duct
- joins with pancreatic duct
- forming ampulla of Vater
- enters duodenum
The top half of the common bile duct is associated with the liver, while the bottom half of the common bile duct is associated with the pancreas, through which it passes on its way to the intestine. It opens in the part of the intestine called the duodenum into a structure called the ampulla of Vater. Blockage of the bile duct by a cancer, gallstones, or scarring from injury prevents the bile from being transported to the intestine and the active ingredient in the bile (bilirubin) instead accumulates in the blood. This condition is called jaundice and the skin and eyes become yellow from the bilirubin in the blood. This condition also causes severe itchiness from the bilirubin deposited in the tissues. In certain types of jaundice, the urine will be noticeably darker, and the stools will be much paler than usual. This is caused by the bilirubin all going to the bloodstream and being filtered into the urine by the kidneys, instead of some being lost in the stools through the ampulla of Vater.Jaundice is commonly caused by conditions such as pancreatic cancer, which causes blockage of the bile duct passing through the cancerous portion of the pancreas; cholangiocarcinoma, cancer of the bile ducts; blockage by a stone in patients with gallstones; and from scarring after injury to the bile duct during gallbladder removal.
Phone Numbers Reach Us -
India & International : +91 9371770341
Diagnosis and Treatment :
Ultrasound scan Sound waves are used to make up a picture of the bile ducts and surrounding organs. These scans are done in the hospital's scanning department. You will be asked not to eat, and to drink clear fluids only (nothing fizzy or milky) for four to six hours before the scan. Once you are lying comfortably on your back, a gel is spread onto your abdomen. A small device, like a microphone, is then rubbed over the area. The sound waves are converted into a picture using a computer. The test is completely painless and takes 15–20 minutes.
CT (computerised tomography) scan A CT scan takes a series of x-rays which are fed into a computer to build up a three-dimensional picture of the inside of the body. The scan is painless but takes from 10 to 30 minutes. CT scans use a small amount of radiation, which will be very unlikely to harm you and will not harm anyone you come into contact with. You will be asked not to eat or drink for at least four hours before the scan. Most people who have a CT scan are given a drink or injection to allow particular areas to be seen more clearly. Before having the injection or drink, it is important to tell the person doing this test if you are allergic to iodine or have asthma. You will probably be able to go home as soon as the scan is over.
MRI (magnetic resonance imaging) This test is similar to a CT scan, but uses magnetic fields instead of x-rays. During the scan you will be asked to lie very still on a couch inside a metal cylinder. The cylinder is a very powerful magnet, so before going into the room you should remove all metal belongings. You should also tell your doctor if you have ever worked with metal or in the metal industry or if you have any metal inside your body (for example, a cardiac monitor, pacemaker, surgical clips, or bone pins). You may not be able to have an MRI because of the magnetic fields. You will usually be given an injection to allow the pictures to be seen more clearly. The test can take about 30 minutes and is completely painless, although the machine is quite noisy. You will be given earplugs or headphones. If you don’t like enclosed spaces you may find the machine claustrophobic. A two-way intercom enables you to talk with the people controlling the scanner.
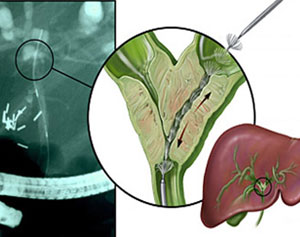
ERCP (endoscopic retrograde cholangiopancreatography) This is a procedure by which an x-ray picture of the pancreatic duct and of the bile duct can be taken. It may also be used to unblock the bile duct if necessary. You will be asked not to eat or drink anything for about six hours before the test so that the stomach and duodenum (first part of the small bowel) are empty. You will be given an injection to make you relax (a sedative) and a local anaesthetic spray will be used to numb your throat. The doctor will then pass a thin flexible tube known as an endoscope through your mouth into your stomach and into the duodenum just beyond it. Looking down the endoscope, the doctor can find the opening through which the bile duct and the duct of the pancreas drain into the duodenum. A dye which can be seen on x-ray can be injected into these ducts and the doctor will be able to see whether there is any abnormality or any blockage in the ducts. If there is a blockage it may be possible or the doctor to insert a small tube known as stent. You may have some discomfort during this procedure; if you do, it is important that you let your doctor know. You will be given antibiotics beforehand (to help prevent any infection) and will probably stay in hospital for one night afterwards.
PTC (percutaneous transhepatic cholangiography) This is another procedure by which your doctor can obtain an x-ray picture of the bile duct. You will be asked not to eat or drink anything for about six hours before the test and will be given a sedative as for the ECRP. An area on the right side of your abdomen will be numbed with a local anaesthetic (an injection) and a thin needle will be passed into the liver through the skin. A dye will be injected through the needle into the bile duct within the liver. X-rays will then be taken to see if there is any abnormality or blockage of the duct. You may feel some discomfort as the needle enters the liver. You will be given antibiotics before and after this procedure (to help prevent infection) and you will stay in hospital for at least one night afterwards.
Angiography As the bile duct is very close to the major blood vessels of the liver, a test called an angiogram may be done. The angiogram can check whether the blood vessels are affected by the tumour. A fine tube is inserted into an artery in your groin and a dye is injected through the tube. The dye circulates in the arteries to make them show up on x-ray. An angiogram is carried out in a room within the x-ray department. Sometimes an MRI scan can be used to show up the blood vessels of the liver and then an angiogram will not be necessary.
Biopsy The results of the previous tests may make your doctor strongly suspect a diagnosis of cancer of the bile duct, but the only way to be sure of the diagnosis is to take some cells or a small piece of tissue from the affected area of the bile duct to look at under a microscope. This is called a biopsy and may be carried out during an ECRP or PTC. A fine needle is passed into the tumour through the skin after the area has been numbed using a local anaesthetic injection. CT or ultrasound may be used at the same time, to make sure that the biopsy is taken from the right place.
Endoscopic ultrasound scan (EUS) This scan is similar to an ERCP but involves an ultrasound probe being passed down the endoscope to take an ultrasound scan of the pancreas and surrounding structures.Cancers of the biliary tract (gallbladder and bile ducts) seldom produce symptoms in the early stages. Patients who develop symptoms of biliary cancer, such as jaundice, will have a physical examination and one or more diagnostic tests. Treatments for bile duct cancer vary with the size of the tumor and how far it has advanced. Among treatments are surgery, liver transplantation, chemotherapy, radiation therapy, photodynamic therapy and biliary drainage. Where the cancer cannot be completely removed but has not spread outside the liver, liver transplantation may be an option. Mayo Clinic is one of the few institutions in the world offering transplantation for bile duct cancer. Read more about treatment for bile duct cancer. Treatments for bile duct cancer vary with the size of the tumor and how far it has advanced. Among treatments are surgery, liver transplantation, chemotherap, radiation therapy, photodynamic therapy and biliary drainage. Where the cancer cannot be completely removed but has not spread outside the liver, liver transplantation may be an option. Mayo Clinic is one of the few institutions in the world offering transplantation for bile duct cancer. Read more about treatment for bile duct cancer.
Complete removal of the tumor is the only effective and potentially curative treatment for cancers of the lower bile duct. The treatment usually requires a Whipple operation. Distal bile duct cancer is more amenable to complete removal compared to pancreatic cancer. Five-year survival rates of up to 40% are found after complete removal of distal bile duct cancer. The type of treatment that you are given will depend on a number of factors, including your general health, the position and size of the cancer in the bile duct and whether the cancer has spread beyond the bile duct.
Consent
Before you have any treatment, your doctor will give you full information about what it involves and explain the aims of the treatment to you. They will usually ask you to sign a form saying that you give permission (consent) for the hospital staff to give you the treatment. No medical treatment can be given without your consent.
Benefits and disadvantages of treatment
Treatment can be given for different reasons and the potential benefits will vary for each person. If you have been offered treatment that aims to cure your cancer, deciding whether to have the treatment may not be difficult. However, if a cure is not possible and the treatment is to control the cancer for a period of time, it may be more difficult to decide whether or not to go ahead. If you feel that you can't make a decision about treatment when it is first explained to you, you can always ask for more time to decide. You are free to choose not to have the treatment and the staff can explain what may happen if you don't have it. You don't have to give a reason for not wanting to have treatment, but it can be helpful to let the staff know your concerns so that they can give you the best advice.
Followup care :
In patients with bile duct tumors, the choice of treatment and the prognosis are influenced greatly by the location of the tumor. Prognosis is better for distal bile duct tumors, histologically differentiated, and polypoidal tumors. Factors that suggest poor prognosis include involvement of lymph nodes, vascular invasion, advanced T stage, positive tumor margins of the resected specimen, and the presence of mutations of P53 gene. With hilar cholangiocarcinoma, the overall resection rate in most series varies form 40-60%. The mean survival rate for patients undergoing curative resection is 67-80% at 1 year and 11-21% at 5 years. Local resection has a lower operative mortality rate (8%) than does major hepatic resection (15%), with a mean survival of 21 months compared with 24 months for major hepatic resection. No clear indication exists that survival is improved significantly by major hepatic resection when compared with local bile duct resection, though some studies suggest that hepatic resection is associated with a greater incidence of tumor-free margins and, consequently, survival. In distal bile duct cancers, the resection rate is more than 60%, and the prognosis is better than for hilar tumors, the mean survival being 39 months. The survival rate varies from 50-70% at 1 year to 17-39% at 3 years.
Diffuse intrahepatic tumors have a dismal prognosis; most patients with these tumors die within 1 year of diagnosis. If left untreated, 50% of patients with bile duct cancer may survive for 1 year, 20% may survive for 2 years, and 10% may survive for 3 years. The role of adjuvant radiotherapy and chemotherapy is controversial. The use of hormones in treatment, including somatostatin analogs, cholecystokinin, and cholecystokinin antagonists, is being investigated. It has been suggested that preoperative endoscopic retrograde cholangiopancreatography (ERCP) with biliary drainage in patients with tumors of the bile duct increases the risk of implantation metastases after resection of the tumor.21 Therefore, preoperative radiotherapy is advocated in such patients, but the benefit has not been definitely proven.22 Transarterial chemoembolization (TACE), infusion of 5-fluorouracil into the hepatic artery or bile ducts, and percutaneous injection of ethanol (PEI) into the lesions are other modalities that are investigational. Photodynamic therapy may be useful in relieving obstruction, especially when obstruction occurs as a result of tumor outgrowth into an endoprosthesis.23 Liver transplantation, when performed for cholangiocarcinoma, is associated with poor surviva
Phone Numbers Reach Us -
India & International : +91 9371770341